Just when you thought you were done learning all the new Evaluation and Management (E/M) Guidelines that were implemented in 2021 and 2023, hold on to your hats …. There are more changes coming. Not to worry though, they are minimal and do not involve a complete overhaul of the way E/M visits are coded.
Looking back.
In 2021, the codes for Office and Outpatient Evaluation and Management went from a system of counting elements under HPI, Physical Exam, and Medical Decision Making to a much-needed change of counting elements strictly related to Medical Decision Making. There was a substantial learning curve, but we made it through. Then a few minor revisions when the scope of guidelines implemented in 2021 was expanded to include the remainder of the E/M codes in 2023.
Let’s just take a moment to rejoice that we no longer have two different sets of guidelines.
What’s changing?
In the 2023 CPT® code book, you were probably shell-shocked to see all the green text under the E/M Guidelines, fear not, you won’t see pages upon pages of green text in the 2024 E/M Guidelines section. There are a few sections that contain new or revised text, but nothing compared to 2023.
Minor Revisions
There are some minor revisions to the E/M Guidelines.
- Clarifying Information can be found on page 8 of the 2024 CPT® Code Book. The added text is not impactful for coding purposes; it is simply just telling us that the definitions of the elements in Table 1 can be found in the guidelines.
- Updated information can be found on page 10 of the 2024 CPT® Code Book. The updated text does help coder understand the term risk as it relates to MDM, telling us when we think about the term risk, it should be in the context of the risk from the condition, and not the management of the condition.
- Clarifying information can be found on page 13 of the 2024 CPT® Code Book. The added text may be impactful for coding purposes, providing an explanation of the high-level assignment for parenteral controlled substances, citing this should be considered when there is a thought process of prescribing parenteral controlled substances, and not just an order being present, so, in other words, there must be documentation to somehow indicate the providers’ decision-making process in ordering a parenteral controlled substance.
Changes in Selecting Levels Based on Time
The big change for 2024 will be the selection of a level based on time. Prior to the upcoming year, the level of service when based on time was selected for time that fell in between a set timeframe, such as 15-29 minutes, in 2024, this has changed to a set time limit that must be met or exceeded.
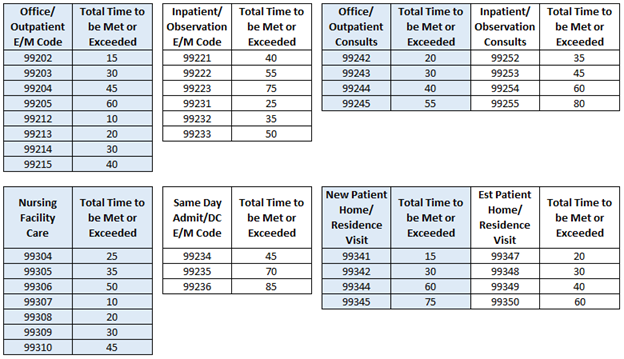
- For example, in 2023, 99202 required 15-29 minutes of total time spent on the date of the encounter; in 2024, 99202 requires 15 minutes of time must be met or exceeded.
Certain E/M sections and code levels have new time constraints which need to be met or exceeded, as shown in the figure below.
There is additional clarifying information on page 13, which is new, regarding leveling services based on time, when determining what can be used as distinct time. In the context of prolonged services, the mid-point between levels does not apply, the full 15 minutes is required to report these services.
Additionally, it is expanded to say when coding based on time, if both the physician and other QHP both take part in the visit, the amount of time personally and individually spent by the provider(s), should be documented to indicate the amount of time spent on face-to-face activities such as managing, counseling, educating and communicating with the patient, and non-face-to-face activities, such as reviewing prior records, historical information, and test results. Any time spent jointly with the patient, should only be recorded once.
Split or Shared Visits
There are changes in the 2024 CPT® book, feel free to review page 6 of the 2024 CPT® Code Book for the guidelines relating to this topic. Succinctly, the most notable change is the definition of substantive portion, stating the provider that has made and/or approved the management of the plan, takes responsibility for the risk, AND has performed 2 of the 3 elements of the MDM would be considered the billing provider. Much to our surprise, CMS has indicated they are going along with the definition CPT® has provided for substantive portion due to the changes of E/M leveling. To read more about this final ruling, please visit the CMS website.
Multiple Evaluation and Management Services on the Same Date
New for this year are guidelines on how to code multiple services provided on the same date. While this isn’t a new concept, the guideline is one we have always wondered about, maybe even billed it before, and now we have official guidelines. It is important to note, these are CPT® guidelines and payers may not accept these concepts, therefore, it is important to check with your payers on their guidelines and/or requirements for billing multiple E/M services that occur on the same date. Here are some of the types of scenarios that may apply to this concept:
- Per day – When a patient is seen multiple times in one day, in the same setting (such as a hospital), we are directed to take all documentation into consideration to determine the final code selection.
- Multiple encounters in different settings – When a patient is seen in two different settings (such as 2 different hospitals) on the same date, an E/M visit can be billed for each facility, however, the documentation must be kept separate and coded as individual encounters, rather than combining them.
- ED and services in other settings (same or different facilities) – If the ED visit is not being reported separately, the total time spent for the day would be combined to determine the final code selection.
Please refer to page 6 of the 2024 CPT® Code Book for the guidelines relating to this topic.
Please note Current Procedural Terminology (CPT®) is copyright 1966, 1970, 1973, 1977, 1981, 1983-2023 by the American Medical Association. All rights reserved.
LW Consulting, Inc. (LWCI) offers a comprehensive range of services that can assist your organization in maintaining compliance, identifying trends, providing education and training, or conducting documentation and coding audits. For more information, contact LWCI to connect with one of our experts!

