The Patient-Driven Payment Model (PDPM) is the reimbursement methodology for Medicare Part A that has been implemented for Skilled Nursing Facilities (SNFs) since October 1, 2019. The PDPM was designed to improve the accuracy of Medicare reimbursement to SNFs by basing the payment on the patient’s clinical characteristics and care needs rather than on the therapy minutes provided. PDPM has complexities that should be considered.
To ensure accurate reimbursement, it is imperative to correctly code the Minimum Data Set (MDS) based on the documentation. It is equally important to enter the information in the appropriate section or item in the MDS. The PDPM is divided into five components: Physical Therapy (PT), Occupational Therapy (OT), Speech-Language Pathology (SLP), Nursing, and Non-Therapy Ancillary (NTA) – and each component has MDS sections or items that need to be appropriately coded for the reimbursement to be accurate.
It is recommended that these resources be utilized to obtain accurate and up-to-date information. Please refer to these resources for any relevant information.
- The Centers for Medicare & Medicaid Services (CMS) – Patient-Driven Payment Model
- Long-Term Care Facility Resident Assessment Instrument (RAI) 3.0 User’s Manual, Version 1.18.11, October 2023
- CMS ICD-10-CM Official Guidelines for Coding and Reporting FY 2024 (October 1, 2023 – September 30, 2024) – Updated October 1, 2023
One PDPM pitfall is the appropriate coding of Respiratory Failure in MDS Section I – Active Diagnoses. LWCI auditors still often find coding errors related to the diagnosis of respiratory failure.
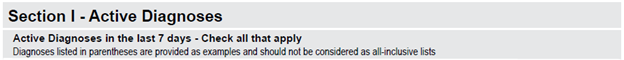
- If a patient has an active diagnosis of Respiratory Failure according to the physician’s documentation, it is important to check MDS item I6300 for Respiratory Failure.
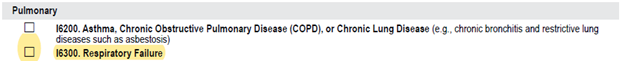
To ensure accurate reporting for MDS Section O – Special Treatments, Procedures, and Programs provided “While a Resident” of your facility; the RAI Manual, Chapter 3, Section O coding instructions for “While a Resident” state:
- “Check all treatments, procedures, and programs that the resident received or performed after admission/entry or reentry to the facility and within the last 14 days. If no treatments, procedures or programs were received by, performed on, or participated in by the resident within the last 14 days or since admission/entry or reentry, check Z, None of the above.”
For example, if a patient at your SNF has a physician’s order for Oxygen as needed due to shortness of breath, and the patient is given Oxygen on the fourth (4th) day of their stay at the SNF, and the Assessment Reference Date (ARD) for the 5-day MDS is on Day 6 of the SNF stay – it is appropriate to code MDS item O0110C1b Oxygen therapy while a resident. This ensures accurately capturing the treatment provided within the 5-day MDS lookback period.
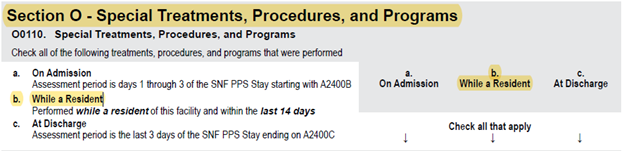
Patients who have been coded with both I6300 Respiratory Failure and O0110C1b Oxygen therapy while a resident may fall under the nursing classification group, Special Care Low, for the PDPM Nursing component. Note this classification applies only if the patient did not receive any of the services or has any of the conditions listed under the nursing classification groups Extensive Services or Special Care High.
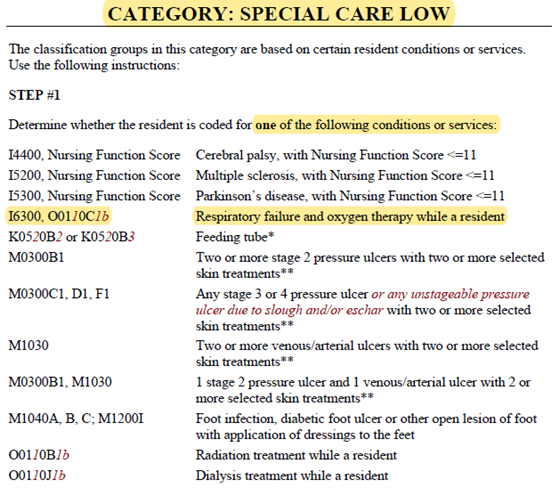
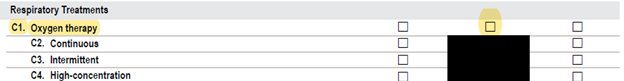
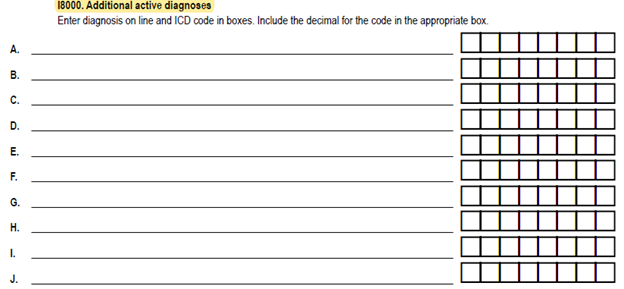
If a patient has an active diagnosis of Respiratory Failure, it is not enough to check item I6300, Respiratory Failure. The specific Respiratory Failure diagnosis must also be listed in I8000, Additional active diagnoses, based on the physician’s documentation about the type of Respiratory Failure.
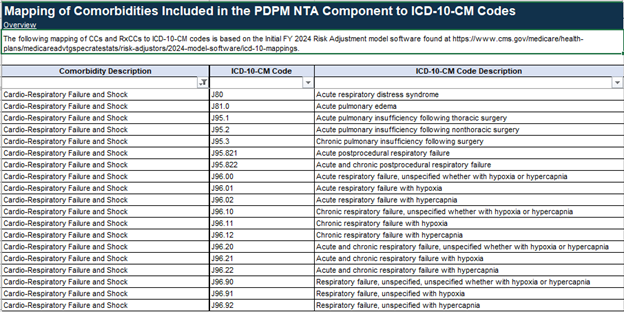
- It is important to ensure that the physician’s note(s) has all information within the lookback period. If any information is missing, it is best to ask the physician and have it documented in the medical record to identify the specific Respiratory Failure ICD-10 diagnosis. This is crucial because it may impact capturing 1 NTA point if this diagnosis falls under the Cardio-Respiratory Failure and Shock comorbidity condition.
NTA Mapping of Cardio-Respiratory Failure and Shock comorbidity condition.
The final review of the MDS coding and documentation is the Triple Check meeting. It is of great importance that SNFs demonstrate accuracy in their coding of the MDS to ensure appropriate Medicare reimbursement. Any inaccuracies in coding could result in over- or under-coding, leading to potential risks, Medicare audits, and inaccurate reimbursement. Therefore, SNFs should consider providing staff regular training and ongoing education to prevent coding errors, promote accuracy, and ultimately lead to appropriate Medicare reimbursement.
Want to continue reading our blog series on PDPM? You can find blog #2 here & blog #3 here.
LW Consulting, Inc. (LWCI) offers a comprehensive range of services that can assist your organization in maintaining compliance, identifying trends, providing education and training, or conducting documentation and coding audits. For more information, contact LWCI to connect with one of our experts!


